Temporomandibular joint disorders (TMJD) can profoundly impact daily activities due to pain and dysfunction in the jaw joints and muscles.
Temporomandibular disorders affect the jaw muscles, soft tissue, and joints, leading to symptoms like jaw pain, facial pain, and difficulty in jaw movements.
Understanding the Temporomandibular Joint
The TMJ is located in front of each ear and connects the mandible (lower jaw) to the temporal bone of the skull.
This joint functions like a sliding hinge, and its unique structure allows for the complex motions required for mouth closure, opening, and lateral movements.
The TMJ is made up of several parts: the condyle, the articular disc, and the articular eminence.
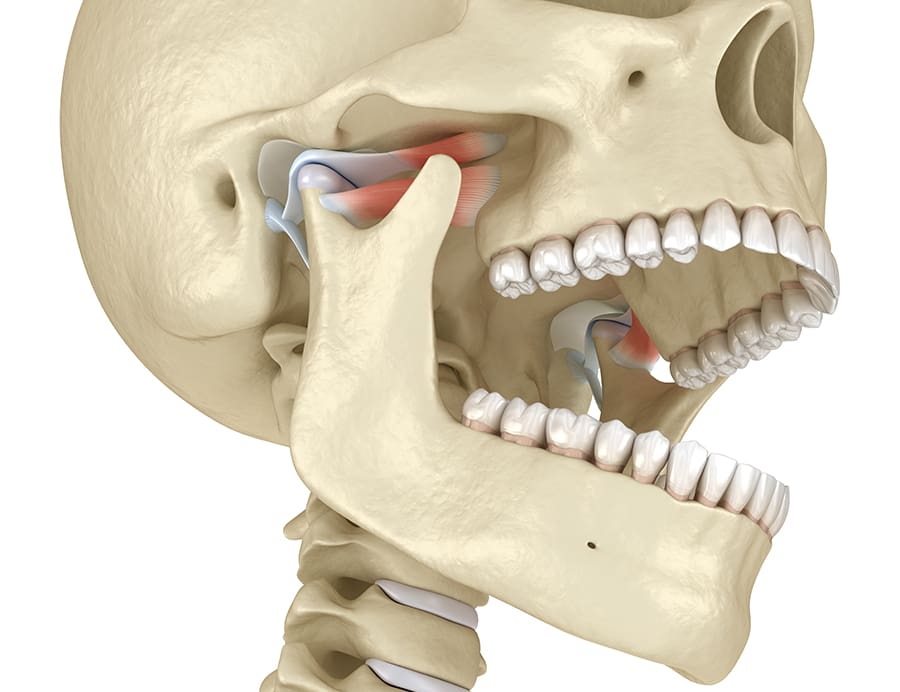
The condyle is the rounded end of the mandible that interacts with the temporal bone. The articular disc is a firm, oval piece of cartilage that cushions the joint movements and minimizes the friction and wear between these bones.
The articular eminence, a bony bump on the temporal bone, guides the movement of the condyle.
Supporting these structures are muscles, ligaments, and a fibrous capsule that surrounds the joint. These structures provide stability and allow smooth joint motion.
These joints usually go unnoticed, performing their duties each day with minimal discomfort. But problems can arise when your chewing muscles and these joints are overworked, damaged or if your bite is misaligned.
Key Takeaway
The temporomandibular joint plays an important role in daily activities like eating, talking, and facial expressions. Inflammation of the joint and the surrounding structures can lead to TMJ disorders.
Causes of TMJ Disorder
TMJ disorders stem from a combination of factors.
Some of the most common causes include:
- Teeth grinding and clenching (bruxism)
- Rheumatoid arthritis
- Jaw injury or dislocation
- Stress
- Malocclusion (bite problems)
Symptoms of TMJ Disorder
TMJ disorder symptoms vary from person to person, depending on the underlying cause.
Some people may experience mild discomfort, while others can have more severe pain that disrupts their daily life.
Some of the most common TMJ disorder symptoms include:
- Jaw pain and tenderness.
- Clicking or popping sounds when opening or closing the mouth.
- Difficulty chewing or opening the mouth fully.
- Earaches, headaches, and facial pain.
- Locking of the jaw joint, making it difficult to open or close the mouth.
Consult a TMJ specialist if you experience any of these symptoms or if they persist over time.
Symptom Checklist: Assessing TMJ Disorder
To help determine if you are experiencing symptoms associated with TMJ disorder, consider the following points as a guide:
- Are you often aware of involuntarily grinding or clenching your teeth during the day or night?
- Do you regularly wake up with soreness or stiffness in the muscles surrounding your jaws?
- Is recurring headache or neck ache an issue for you?
- Does clenching your teeth seem to intensify the pain you feel?
- Have you noticed a relationship between the levels of stress you experience and increased jaw pain or clenching?
- Does your jaw often make sounds such as clicking, popping, or grating when you open it, and does it ever get stuck in an open or closed position?
- Do you find it challenging or painful to open your mouth widely, or experience discomfort while eating or yawning?
- Have you sustained any injuries to your neck, head, or jaw in the past?
- Have you experienced joint issues such as arthritis elsewhere in your body?
- Are there noticeable changes in how your teeth align when you close your bite?
- Is using your front teeth to bite or tear food difficult?
- Do you have concerns about tooth sensitivity, looseness, fracture, or wear?
If you said ‘yes’ to some or all of these questions, you should consult with a TMJ disorder specialist for an evaluation.
Non-Surgical Treatment Options
We offer comprehensive evaluations and personalized treatment plans for TMJ disorder. We work closely with patients to find the best solution for their individual needs.
Some non-surgical treatment options for TMJ disorder include:
- Botox® injections: Botox is an FDA-approved treatment that can help relieve muscle tension and pain in the jaw caused by TMJ disorder.
- Nightguard appliances in combination with pharmacotherapy: Nightguards (occlusal guards) help reduce teeth grinding and clenching, while medications can alleviate symptoms like pain and inflammation.
- PRF injections: Platelet rich fibrin (PRF) is a natural treatment option that uses your body’s own healing properties to promote tissue regeneration in the jaw joint.
- Physical therapy and jaw exercises: Stretching and strengthening exercises can help improve jaw muscle function and relieve tension.
- Stress management techniques: Stress is a common trigger for TMJ disorder. Learning stress management and relaxation techniques can help decrease symptoms.
Botox® for TMJ Disorder
Botox injections are an increasingly popular option for managing TMJ disorder symptoms. Botox works by temporarily paralyzing the muscles responsible for jaw tension, reducing pain and allowing the jaw to relax.
The procedure involves injecting small amounts of Botox into specific areas of the jaw muscles, targeting trigger points that are causing discomfort. The number of units used varies depending on individual needs.
Patients may experience some mild side effects like bruising or swelling at the injection site, but these usually subside within a few days.
Surgical Treatment for TMJ Disorder
If non-surgical treatments are not effective or if there is a severe underlying issue causing the TMJ disorder, we may recommend arthrocentesis.
Also known as joint aspiration, arthrocentesis is a minimally invasive procedure that involves flushing out the joint with a sterile solution to remove debris and inflammatory fluids.
This is followed by the injection of a special sterile solution made up of saline, anti-inflammatory steroids, and collagen components into the TMJ using a single needle. The fluid is pumped under pressure into the jaw joint space to flush out any fluid buildup in the area, while a second needle is used to remove the sterile solution and accumulated fluid.
PRF injections can also be used in conjunction with arthrocentesis to promote healing and restore healthy tissue in the joint.
Daily Habits and Practices to Relieve TMJ Pain
Managing TMJ disorder effectively can often begin with small, daily adjustments and practices that help alleviate pain and discomfort.
Here are several strategies you can incorporate into your routine:
- Jaw relaxation exercises: Practice gentle jaw stretches and relaxation exercises to release tension from the muscles. Consider consulting with a physical therapist for specific exercises tailored to your needs.
- Good posture: Maintain good posture throughout the day to reduce strain on your neck and jaw. Ensure that your work environment is ergonomically set up and take regular breaks to stretch.
- Dietary adjustments: Opt for soft foods that require less chewing, especially during flare-ups. Avoid tough, chewy foods like gum and hard candies that can exacerbate jaw tension.
- Heat and cold therapy: Apply moist heat in the form of a warm towel or hot pack to the jaw area for 10–15 minutes several times a day to ease pain. Alternatively, try cold packs to reduce inflammation and numb acute pain.
- Stress reduction techniques: Incorporate stress management techniques such as meditation, deep breathing exercises, or yoga into your daily routine to minimize clenching and grinding caused by stress.
- Mindful chewing: Pay attention to your chewing habits, making an effort to chew evenly on both sides and avoid clenching your teeth when not eating.
- Regular physical activity: Engage in daily physical activity and exercises that promote overall muscle strength and relaxation, helping to balance stress levels and improve well-being.
- Medication options: Non-steroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and inflammation in the jaw, while muscle relaxants may alleviate muscle tension. Always follow the dosage instructions and consult with a healthcare professional for appropriate recommendations based on your specific situation.
Integrating these practices into your daily life can significantly aid in managing symptoms and promoting a healthier jaw function.
TMJ Consult at Concord Oral Surgery
If you are experiencing symptoms of TMJ disorder, the first step is to schedule a consultation with our team.
Dr. Robert Barron, DMD, will conduct a thorough evaluation and discuss all possible treatment options to help alleviate your pain and improve jaw function.
We specialize in treating various dental problems, including wisdom teeth removal and dental implants. Talk to us about your concerns, and we’ll provide you with personalized solutions to meet your unique oral health needs.
If you have any questions or concerns regarding your oral health, please reach out to us to schedule a consultation. To book an appointment at our oral surgery office in Vaughan, call (905) 669-2616 or complete the appointment request form.
FAQs About Temporomandibular Joint Disorders
What is the difference between TMJ and TMD?
TMJ refers to the temporomandibular joint itself, while TMD stands for temporomandibular joint disorder. TMJ is a part of the body, while TMD is a condition that affects the joint and surrounding muscles.
Can braces fix TMJ?
Braces can be an effective treatment for TMJ disorder in some cases. However, it’s best to consult with a dental professional to determine the underlying cause of your TMJ and develop a personalized treatment plan.
How many units of Botox are needed to treat TMJ?
The number of units used in Botox injections for TMJ disorder can vary depending on individual needs, but it typically ranges from 60-100 units per side.
Does Botox for TMJ change face shape?
Botox injections for TMJ do not change the shape of your face. However, the muscles that the Botox is injected in will be temporarily paralyzed, so they may decrease in size over time.
Where is Botox injected for TMJ?
Botox is typically injected into the masseter, temporalis, and occasionally into the lateral pterygoid muscles. The masseter is located at the angle and lateral surface of the jaw and is responsible for chewing, the temporalis is situated on the side of the head and helps in closing the jaw, while the lateral pterygoid muscle is responsible for protruding the mandible and it is attached onto the articular disc and the capsule of the temporomandibular joint.